Spasticity in MS (Multiple Sclerosis)

Spasm and stiffness in multiple sclerosis
When multiple sclerosis affects motor areas of the central nervous system, it can impact connections between the brain and muscles, causing muscles to feel rigid or stiff or to spasm and jerk involuntarily.
Muscle tightness and jerking are common among people living with multiple sclerosis, with symptoms ranging from mild to severe. Some mild muscle stiffness can actually be beneficial for people with leg weakness, making it easier to stand and walk, but it still needs to be managed. If these symptoms sound familiar to you, read on to learn more about how they can impact people living with multiple sclerosis and how they are managed and treated.
2.8M
people
worldwide live with multiple sclerosis1
86%
of people
with multiple sclerosis have some form of spasticity2
85%
of people
with multiple sclerosis present with the relapsing-remitting form3

Measuring spasticity
The impact of spasticity can be measured using the Ashworth Scale, which can be used to:

Assess resistance to passive stretching

Measure muscle tone using a five-point scale (six in the modified version)

Assess the impact on a person’s ability to move around and their independence
Differentiate between mild and severe spasticity
What is multiple sclerosis?
Multiple sclerosis (MS) is believed to be an autoimmune disease, caused by the immune system attacking healthy tissue in the central nervous system (the brain, spinal cord, and optic nerves). When the insulating layer that protects nerve fibers (called myelin) is damaged, it can lead to inflammation that blocks the passage of nerve signals and causes messages from the brain to be slowed or lost. This, in turn triggers the symptoms of multiple sclerosis, including cognitive difficulties, vision problems, movement difficulties, fatigue, muscle weakness and tightness, and spasms.
There are four types of multiple sclerosis, classified by disease activity and progression:
- Clinically isolated syndrome (CIS)
- Relapsing-remitting multiple sclerosis (RRMS)
- Secondary-progressive multiple sclerosis (SPMS)
- Primary-progressive multiple sclerosis (PPMS).4
In relapsing-remitting multiple sclerosis, symptoms suddenly come and go, or worsen, during periods of relapse (also known as flare-ups or exacerbations), which can last for a few days, weeks, or months. In the progressive forms of the disease, symptoms gradually worsen over time.

Recognizing spasticity in multiple sclerosis
While spasticity in multiple sclerosis can go unnoticed, it´s important to recognize the signs and symptoms to be able to manage and treat the condition effectively.
Is it spasticity?
Feelings of inflexible or tight muscles, as well as problems with jerking and kicking movements in multiple sclerosis, are all symptoms of a condition known as spasticity. Spasticity looks and feels different for everyone, but there are some common symptoms to watch out for.
Various signs to look for
- Muscles that feel stiff, tight, rigid, numb, heavy, or paralyzed
It can be difficult to bend or straighten your arms, legs, fingers, or other parts of the body - Spasms
Involuntary jerking or kicking movements, or uncontrolled bouncing, tremors, twitches, or shakes - Muscle twitching and jerking
Getting worse at night, interrupting sleep - Pain or tightness around the joints
As well as lower back pain - Movement difficulties
Making it difficult to walk, balance, or stand up straight
What can trigger spasticity in multiple sclerosis?
Like other symptoms of multiple sclerosis, muscle rigidness and spasms can flare up during a period of relapse. Different trigger factors (including changes in your environment or routine) can worsen or exacerbate problems with muscle tightness and jerking, so it’s useful to try and identify these trigger factors to effectively manage symptoms and minimize their effects. Triggers are different for each person, so you’ll need to work with your healthcare team to track your symptoms and identify possible triggers for you. Triggers could include:
- Other multiple sclerosis symptoms, such as bowel or bladder dysfunction
- Sudden movements, position changes, or lack of movement
- Fatigue or time of day, often at night
- Temperature changes
- Infections or injuries
- Tight clothing
- Skin irritation or pressure sores
- Emotional stress
Spasticity treatment and exercises for people with multiple sclerosis
Left untreated, muscle stiffness can cause contractures (frozen joints) and pressure sores. Both muscle tightness and spasms can be treated through exercises – stretching, range-of-motion, and relaxation – along with physical therapy, hydrotherapy, massage, and orthoses.
Medical interventions such as botulinum neurotoxin can also help. Your multidisciplinary specialist team will work with you to develop a personalized treatment and exercise plan to manage your symptoms and trigger factors.




References
1. Walton C, King R, Rechtman L, et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Mult Scler. 2020 Dec;26(14):1816-1821.
2. 2. Milinis K, Tennant A, Young CA; TONiC study group. Spasticity in multiple sclerosis: Associations with impairments and overall quality of life. Mult Scler Relat Disord. 2016 Jan;5:34-9.
3. McKay KA, Kwan V, Duggan T, Tremlett H. Risk factors associated with the onset of relapsing-remitting and primary progressive multiple sclerosis: a systematic review. Biomed Res Int. 2015 Jan; 2015:817238.
4. Lublin FD, Reingold SC, Cohen JA, et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. 2014 Jul;83(3):278-286.
Spasticity after stroke

What causes post stroke spasticity?
After a stroke, it is quite common for people to be left with muscle weakness and stiffness. It can feel as though the muscles are pulling and tight and can contract involuntarily. This is called post-stroke spasticity.
While there are no cures for post-stroke spasticity, this condition does not progressively worsen. In fact, it can be treated with a tailored rehabilitation program, which can help the often frustrating and painful symptoms improve over time.
Understanding stroke
Stroke happens when the blood supply to the brain is blocked, either by a blood clot (ischemic stroke) or burst blood vessel (hemorrhagic stroke). Starved of oxygen, brain cells die, leading to a range of symptoms depending on where in the brain the stroke has occurred. The resulting brain damage can leave stroke survivors with lasting impacts such as speech problems and impaired mobility, as well as impacts on cognition and mental health.
The quicker a stroke is detected and treated, the quicker blood flow can be restored to the brain – thereby reducing damage to the brain. Emergency treatment in hospital can remove or dissolve blood clots in the brain, while specialist acute stroke care can improve outcomes and help prevent a second stroke. Early rehabilitation in hospital, such as physical therapy and speech and language therapy, can help stroke survivors recover skills and functions that may have been impacted. This type of support is vital in the weeks and months following a stroke.
1 in 4
adults
over the age of 25 will have a stroke in their lifetime1
110M
people
in the world have experienced stroke1
87%
of strokes
are ischemic strokes2
45%
of stroke survivors
can expect to develop spasticity within 3 months3

Effects of stroke
Stroke can lead to psychological, physical, cognitive, and communication problems, including:
- Neurological deficits – tingling, numbness, a drooping mouth, or facial paralysis
- Cognitive issues – difficulties with concentration, memory loss, hearing, spatial awareness, and comprehension
- Fatigue
- Impaired speech (aphasia)
- Vision problems
- Mental health challenges – anxiety and depression
- Lack of body control – muscle weakness, tightness, or spasms
Stroke and spasticity
Upper Motor Neuron Syndrome
When someone has a stroke, the part of the brain that controls voluntary movement can be damaged. This is known as Upper Motor Neuron Syndrome. On the one hand, this damage can be described by what is lost: motor skills, strength, or motor control, for example. On the other hand, it can be characterized by continuous and unwanted muscle activity – uncontrollable movements, spasms, or involuntary muscle contractions.
Measuring spasticity
The impact of spasticity can be measured using the Ashworth Scale, which is used to:
- Assess resistance to passive stretching
- Measure muscle tone using a five-point scale (six in the modified version)
- Assess the impact on a person’s ability to move around and their independence
- Differentiate between mild and severe spasticity
Recognizing spasticity after stroke
While spasticity after stroke can go unnoticed, it´s important to recognize the signs and symptoms to be able to manage and treat the condition effectively.
Is it spasticity?
Post-stroke spasticity can be difficult to recognize among other symptoms and can be overlooked in early or mild stages. Spasticity looks and feels different for everyone, but there are some common symptoms to watch out for.
Signs to look for
- Muscles that feel stiff, tight, rigid, numb, heavy, or paralyzed
Making them resistant to movement or difficult to bend or straighten through a full range of motion - Muscle weakness or paralysis
Affecting one side of the body (known as hemiparesis) - Muscles remaining “frozen” or “locked” in certain positions
Such as an elbow bent against the chest, a clenched fist, or pointed toes - Spasms
Involuntary jerking or kicking movements, or uncontrolled bouncing, tremors, twitches, or shakes - Movement difficulties
Makting it difficult to walk, balance or stand up straight - A lack of body control that makes it hard to complete daily tasks
Such as getting dressed, cooking, and cleaning

Treatment and rehabilitation exercises for post-stroke spasticity
Detailed clinical and neurological assessments by stroke specialist rehabilitation teams can help to determine a personalized treatment plan. Goals can include everything from relieving pain and improving mobility to resuming everyday activities or gaining more independence.
Treatment can include physical, occupational, and speech therapies (many stroke survivors report that they continue to see improvement even after many months of therapy). Mobility aids, assistive technologies (orthoses), and medical interventions such as botulinum neurotoxin can also help to reduce spasticity symptoms. At-home exercises are also important to improve mobility and reduce acute muscle tightness.
References
1. GBD 2016 Lifetime Risk of Stroke Collaborators, Feigin VL, Nguyen G, et al. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N Engl J Med. 2018;379(25):2429-2437.
2. Virani, SS, et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021; 143(8), e254–e743.
3. Schinwelski MJ, Sitek EJ, Wąż P, Sławek JW. Prevalence and predictors of post-stroke spasticity and its impact on daily living and quality of life. Neurol Neurochir Pol. 2019; 53(6):449-57.

How everyday life changes with post-stroke spasticity
With spasticity many aspects of everyday life can be difficult and arduous and sometimes even become extremely challenging. The following areas may be affected:
- Eating and cooking
- Dressing
- Housekeeping
- Mobility (walking to the supermarket or to work)
- Sleep quality
- Personal hygiene
- Posture
Depending on the location and extent of the spasticity these effects can range from mild impairment of activities of daily living to severe limitations in patients’ private and professional lives.
Patients may need help with activities that they could previously do naturally and completely independently. These might be very personal or intimate activities, such as daily hygiene, preparing a meal or getting dressed. Patients may also find it difficult to pursue their careers as usual or indeed at all.
There are better and worse days. But nevertheless I welcome every single day, because each one of them might bring something good and unexpected.

Support is key: Post-stroke spasticity patients must not be left to cope alone.
Specialist doctors, physiotherapists and occupational therapists as well as self-help organizations are always on hand to give help and advice. Although not curable, with the research and development of modern treatment methods and their application spasticity is now easily treatable. Often treatment can ease patients’ symptoms to such an extent that they can resume their everyday activities and largely regain their quality of life.
The aim of this page is to help patients, family members, carers and interested parties to get in touch with specialists, other patients and helpers, who will encourage them and help them pick up their normal daily lives again.
Spasticity – who can help me?

Make an appointment with your GP:
They can refer to you neurology specialists and physiotherapists.

Patient communities:
Talk to other people who live with spasticity. You can share experiences and encourage each other.

Care Managers:
Specialist carers are trained to help you get back to work and resume your everyday life.

55 – How important are people around you after a stroke?
In the 55th video of the video campaign Kasia describes what the post-stroke experience is like, especially when it comes to friends and how to deal with it. It is very difficult for both sides, but it would be very helpful and also nice to know that you can rely on friends and family.

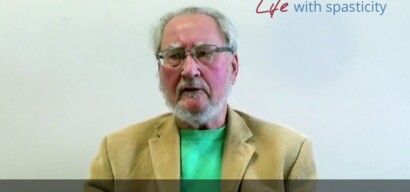
9 – Do you have any advice for stroke survivors with spasticity?
In the ninth episode of our video campaign David Britt talks about his advice for stroke survivors who are experiencing post-stroke spasticity to get involved and seek advice from specialists.
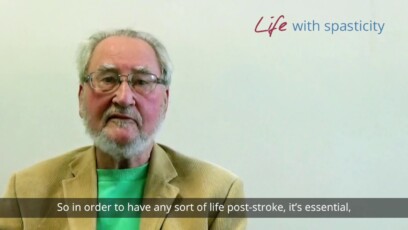
12 – Did your caregiver/relative support you in the way you needed?
In the twelfth episode of our video campaign David Britt describes the importance of familiar support to deal with a stroke.
19 – What advice would you give to stroke survivors?
You need some advice by stroke patients? Listen to David Britt in our nineteenth video of our video campaign. He speaks about his personal experiences dealing with the stroke.
21 – What advice would you give to carers of stroke survivors
In our twenty-first video of our video campaign an old acquaintance, David Britt comes back. He collects many useful hints for carers of stroke survivors.

56 – How helpful are support groups?
In the 56th video of the video campaign Kassia tells about the support groups and that there is no offline group in her city, but that you can also use social media groups and no question is left unanswered.

57 – How important is it to keep hope alive?
In the 57th video of the video campaign Kasia mentions how important it is to have hope. Hope to herself and to others. It is also nice for her to see that in a group all are happy for others when someone has made it and was successful.